Exploring the Different Types of Myelodysplastic Syndromes
Discover how identifying your specific type of Myelodysplastic Syndrome (MDS), including its genetic factors, can guide treatment strategies and influence prognosis.
Classifying myelodysplastic syndromes (MDS) is essential for accurate diagnosis, effective treatment planning, and improving patient outcomes.
MDS, also known as myelodysplastic neoplasms, represent a group of uncommon blood cancers that originate in the bone marrow’s blood-forming cells. These syndromes result in the excessive production of abnormal, immature blood cells that hinder the development of healthy red blood cells, white blood cells, and platelets.
While some MDS cases can progress to acute myeloid leukemia (AML), this progression is not universal, which is why the older term 'pre-leukemia' is now rarely used.
In 2022, the World Health Organization (WHO) updated its tumor classification system, including new categorizations for MDS.
Knowing your specific MDS type helps healthcare providers predict disease progression and tailor treatment approaches effectively.
Here’s a detailed overview.
How Are Myelodysplastic Syndromes Classified?
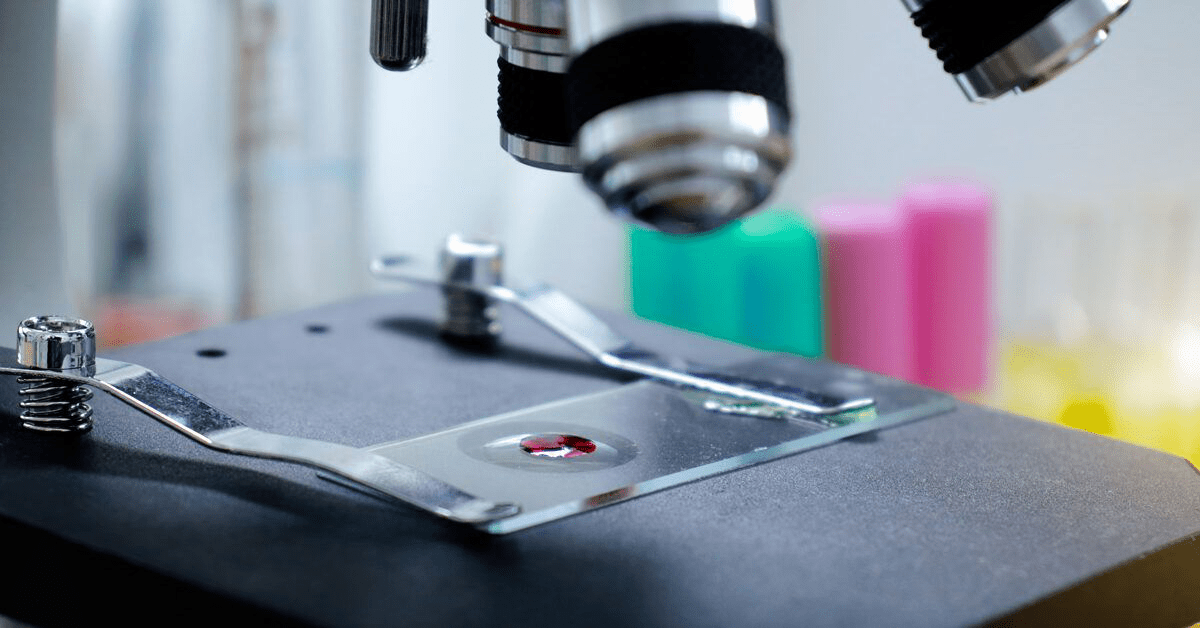
MDS classification is based on microscopic examination of blood and bone marrow cells combined with genetic analyses. Key factors considered include:
- Counts of white blood cells, red blood cells, and platelets
- Proportion of abnormal cells observed under the microscope
- Chromosomal abnormalities detected in bone marrow cells
- Percentage of immature and abnormal cells in blood and marrow
- Presence and quantity of ring sideroblasts—abnormal red blood cell precursors with iron deposits
Main Types of Myelodysplastic Syndromes
The 2022 WHO guidelines categorize MDS into two primary groups: genetic-based and morphology-based types.
Genetic-Based MDS Categories
These types are defined by specific genetic mutations or abnormalities.
MDS with Low Blasts and Isolated 5q Deletion (MDS-5q)
This subtype involves deletion of a segment of chromosome 5 in bone marrow cells, without loss of chromosome 7. It typically features low counts of one or two blood cell types, most often red blood cells, alongside an increase in certain abnormal blood cells.
MDS-5q is uncommon, predominantly affects older women, and generally has a favorable prognosis with a low risk of progression to AML.
MDS with Low Blasts and SF3B1 Mutation (MDS-SF3B1)
A newer classification replacing the former MDS with ring sideroblasts (MDS-RS), this type involves a mutation in the SF3B1 gene and a low percentage of ring sideroblasts. It accounts for over 90% of MDS cases previously categorized with ring sideroblasts.
MDS with Biallelic TP53 Inactivation (MDS-biTP53)
This subtype is characterized by mutations that inactivate both copies of the TP53 gene, which plays a crucial role in regulating cell division. Approximately 11% of MDS patients exhibit pathogenic TP53 mutations, with many having multiple alterations.
Morphology-Based MDS Categories
These types are defined by the structural characteristics of the affected cells.
Hypoplastic MDS (MDS-h)
MDS-h is a newly recognized subtype marked by reduced bone marrow cellularity due to immune system attacks on marrow renewal cells and increased inflammatory cytokines. It shares features with conditions like aplastic anemia and paroxysmal nocturnal hemoglobinuria, requiring thorough morphological analysis for accurate diagnosis.
MDS with Low Blasts (MDS-LB)
This type is characterized by a low number of ring sideroblasts in the bone marrow and bloodstream.
MDS with Increased Blasts (MDS-IB)
Defined by an elevated number of ring sideroblasts and decreased counts of at least one blood cell type, MDS-IB can be further divided into:
- MDS-IB1
- MDS-IB2
- MDS with Fibrosis (MDS-f)
Primary vs. Secondary Myelodysplastic Syndrome
Primary MDS occurs without a known cause and is the more common form. Secondary MDS develops due to identifiable factors, such as prior chemotherapy, radiation exposure, smoking, or long-term contact with chemicals like benzene.
Secondary MDS is rarer and generally less responsive to treatment.
Assessing Prognosis and Risk of AML Transformation
The Revised International Prognostic Scoring System (IPSS-R) is widely used to evaluate overall survival and the likelihood of MDS progressing to AML. It scores patients from 1 to 5 based on:
- Presence of genetic abnormalities
- Bone marrow blast percentage
- Severity of cytopenias
The IPSS-R score also guides treatment decisions. Emerging molecular-based scoring systems are under investigation but require further validation.
Individual prognosis varies depending on health status, age, MDS subtype, and treatment response. Consulting with your healthcare team is essential for personalized guidance.
Summary
Myelodysplastic syndromes are blood cancers characterized by excessive immature blood cells and reduced healthy blood cell counts. Classification relies on cellular appearance and genetic features.
Identifying your MDS subtype empowers your medical team to forecast disease progression and customize your treatment plan for optimal outcomes.
Discover engaging topics and analytical content in Sexual Wellness as of 21-10-2023. The article titled " Exploring the Different Types of Myelodysplastic Syndromes " provides new insights and practical guidance in the Sexual Wellness field. Each topic is meticulously analyzed to deliver actionable information to readers.
The topic " Exploring the Different Types of Myelodysplastic Syndromes " helps you make smarter decisions within the Sexual Wellness category. All topics on our website are unique and offer valuable content for our audience.